Why Leading Practices Are Switching to ScribeEMR’s 2026 Medical Scribing Services – And What the Future Holds
Why Leading Practices Are Switching to ScribeEMR’s 2026 Medical Scribing Services – And What the Future Holds
Healthcare was never meant to run like this. Physicians chasing charts late at night. Clinics overwhelmed by admin queues. Patient conversations turning into keyboard notes. The challenge for independent and rural practices today isn’t clinical skill – it’s time, accuracy, and sustainable operations.
Industry surveys show that primary-care physicians spend nearly twice as many hours documenting EHR notes as they do with patients.¹ Burnout rates among clinicians remain persistently high, largely tied to documentation overload and administrative burden.²
For smaller practices, this also leads to delayed charting, lower patient throughput, and avoidable claim denials from inconsistent or rushed notes.³
As the industry shifts toward smarter workflows, 2026 Medical Scribing Services are becoming essential for practices seeking efficiency, accuracy, and long-term stability. With ScribeEMR supporting 1,000+ providers over 7+ years, one conclusion is clear: practices don’t just need scribes – they need the right scribing partner built for the future of modern healthcare.
ScribeEMR: 2025 Impact Snapshot
| Metric | Without a Scribe | With ScribeEMR | Impact Category |
| Daily patient volume | ~20/day | 24–28/day | Higher throughput⁴ |
| After-hours charting | 2–3 hrs/night | <30 min/day | Nights reclaimed⁴ ⁵ |
| Denials tied to documentation | Baseline | ↓ 30–40% | Cleaner claims⁶ |
| Note accuracy | Manual variability | 98%+ (internal audits) | Better documentation⁴ |
| Physician burnout | 50–63% reported¹ ² | ↓ 21.2% absolute reduction | Lower burnout² |
| Weekly time saved | – | 10–15 hrs/provider | More personal life⁴ |
AI Medical Scribing + Human Review: 2025’s Big Shift
While traditional scribing remained valuable, 2025 marked a major transformation with the adoption of hybrid AI systems – ambient AI drafts, followed by human review and final structuring.
Studies show that AI-assisted medical documentation captures up to 99% of clinician-patient dialogue with high contextual accuracy, allowing human scribes to shift focus to quality polish instead of manual entry.⁷ Hybrid scribing models significantly outperform pure AI systems by improving template alignment, reducing hallucinations, and preserving clinician preference patterns.⁸ ⁹
ScribeEMR’s AI solution, ScribeRyte AI, enabled:
- Real-time ambient note generation, synced into clinician workflows
- Document-first drafts that are later refined by human scribes
- Faster sign-off, lower error correction, and better narrative consistency⁴ ⁸
In 2025, this human + AI combination proved decisive for practices using top enterprise EHR platforms such as Epic Systems and athenahealth where structured documentation quality directly impacts coding and claims.⁴ ⁶ ⁸
AI didn’t replace scribes – it elevated what scribes could do.
From burnout to better workflows – Client testimonial:
“ScribeRyte has completely changed how I finish my day. I used to spend hours after clinic documenting - now when clinic ends, I’m done. The turnaround is fast, the note quality is excellent, and the team truly tailors documentation to how I practice. I see 40–60 patients a day and the system makes me more efficient without slowing me down.” To know more - Watch the video
More Than Notes: 2025’s Expanded Scope
Independent practices increasingly started adopting operational support that could scale beyond documentation.
Many ScribeEMR scribing teams also began:
✅ verifying clinical inbox items
✅ initiating refill drafts
✅ pre-loading patient history
✅ supporting administrative queues in EHR via Virtual Medical Assistant pods⁴
These added efficiencies echo findings that delegating non-clinical administrative burdens to virtual assistant teams significantly improves physician satisfaction and practice resilience.¹⁰
Additionally, 2025 audits by ScribeEMR’s internal RCM teams confirmed that high-quality, structured scribed charts reduced claim denials by 30–40% when combined with professional coding + billing review.⁴ ⁶
Looking Forward: 2026 Medical Scribing Services - A New Standard
If 2025 proved the impact, 2026 is where scaling meets intelligence.
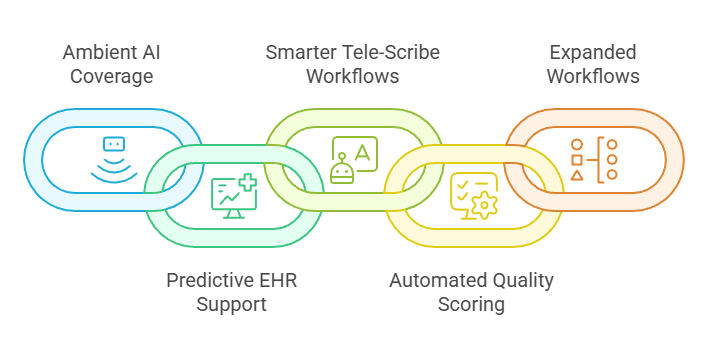
What practices can look forward to:
🔹 Even deeper ambient AI coverage → better conversation-to-chart understanding⁷
🔹 Predictive EHR queue support → auto prioritizing tasks for scribes + VMOS teams
🔹 Smarter tele-scribe workflows → with specialty voice tuning and faster drafts⁷ ⁹
🔹Automated quality scoring of clinical notes before physician sign-off⁷
🔹More workflows beyond charting → referrals, verifications, scheduling, and patient data prep through VMOS + AI pods⁴ ¹⁰
Most importantly, 2026 shifts the promise from “saving time” to **giving clinicians their life back with systems that learn them, support them, and scale like an extension of their clinic.**⁴ ⁷ ⁸
The Real 2025 Outcome? Earlier Evenings, Clearer Claims, Better Care
The stronger the note – the stronger the care and the claim. The faster the chart closes – the better the clinical flow. And when documentation stops consuming clinicians, patient care improves naturally.
2025 wasn’t just a data milestone for ScribeEMR – it was the year practices finally realized documentation support isn’t optional, it’s foundational.
And 2026?
It will be the year that support becomes intelligent, predictive, and truly scalable for every independent and rural provider.
References
- AMA Physician Practice Benchmark 2024
- Medscape Physician Burnout Report 2024
- Annals of Internal Medicine, documentation error impact 2024
- ScribeEMR Internal Client Survey 2025 (1,000+ providers)
- JAMA Study on After-Hours Charting 2024
- ScribeEMR Internal Billing Denial Analysis 2024–2025 (400+ practices)
- arXiv Ambient Clinical Documentation Study 2025
- NEJM Catalyst, Hybrid Scribing Performance 2025
- JAMA Health Forum, AI + Human Documentation Meta-Analysis 2025
- Healthcare Virtual Assistant Delegation Study 2024